Pairing Care and Technology to Increase Optimal Starts
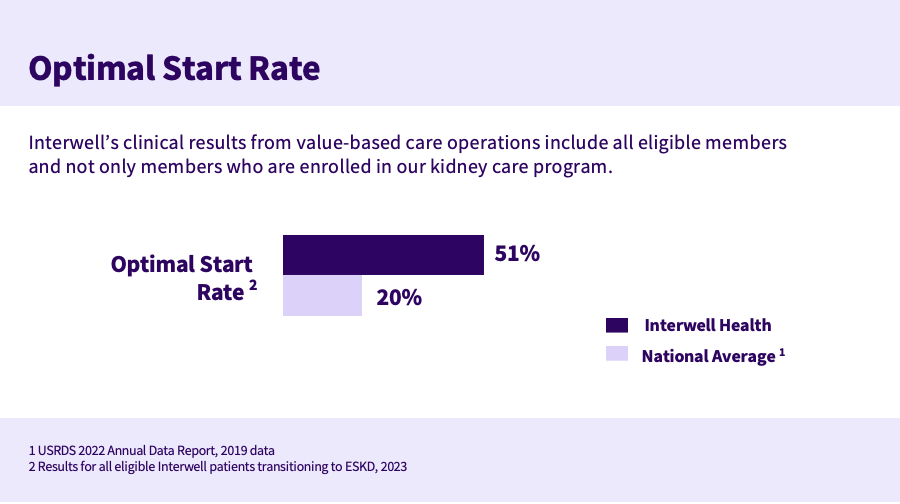
Interwell Health’s care model and provider-centered resources improve the transition to end-stage kidney disease and have resulted in an optimal start rate of 51 percent – 154 percent above the national average.
tags

Consider two patients with late-stage chronic kidney disease.
Jessica is unaware she has kidney disease. She begins dialysis suddenly when abrupt kidney failure sends her to the hospital emergency room. With no time to understand her options and no connection to a nephrologist, Jessica is overwhelmed and anxious. She is also at greater risk of complications -- research suggests an unplanned dialysis start is associated with a higher risk of bloodstream infection, rehospitalization, and mortality.1
Another patient, Ryan, connects with Interwell Health through his health plan after being diagnosed with late-stage chronic kidney disease (CKD). With help from a designated Interwell nurse care manager and a multidisciplinary care team, Ryan learns how to follow a kidney-friendly diet, attends all his nephrology appointments, and works to control his blood pressure. These interventions slow his disease progression and mitigate his risk of unnecessary and costly hospitalization.
Ryan works with his nephrologist and the Interwell team for over a year to prevent kidney failure. Though he is taking effective preventative measures, eventually his kidney function declines to the point that he needs dialysis.
Ryan’s care manager, in close collaboration with his nephrologist, begins modality education so he can understand and consider his treatment options while he is medically stable. He decides he wants to undergo hemodialysis at home and Interwell coordinates his training and permanent access placement. He starts home dialysis feeling competent and prepared and is able to enjoy an improved quality of life.
The benefit of optimal starts
Ryan experienced an optimal start, defined as a person with CKD who transitions to end stage kidney disease (ESKD) by receiving a preemptive transplant, starting peritoneal dialysis, or beginning hemodialysis at home or in center with a permanent access.
Optimal starts benefit patients and healthcare systems and are an important quality measure for Medicare’s KCC Model. They result in improved outcomes and significantly lower costs.2 A recent retrospective study found that optimal starts decrease pre-dialysis cost by $49,168 per patient per year and post-dialysis cost by $16,565 per patient per year when compared to unplanned starts.3
Interwell’s approach
Interwell Health is outperforming the nation in optimal starts for ESKD. Our 2023 optimal start rate for all eligible patients was 51 percent – 154 percent above the national average. We measure these results across all patients with access to our services who need to transition to ESKD.
These results stem from a care model that emphasizes nephrologist partnership, patient education, and provider-centered resources and platforms that enable early intervention and better care coordination.
A planned transition
Achieving optimal starts requires focused care coordination in combination with kidney disease education.
When Interwell Health’s predictive models identify patients at risk of progressing to late-stage CKD, we engage them immediately, before their kidneys fail. Without careful planning these patients will typically begin unplanned dialysis via hospital admission.
“Leveraging predictive analytics, we are able to identify patients at risk for progression,” explained Terry Ketchersid, MD, senior vice president of Interwell. “Those patients receive standardized kidney disease education which empowers the patient and their family to make the best treatment choice for their specific care goals.”
Interwell deploys multidisciplinary care teams — made up of coordinators, nurses, social workers, and renal dietitians — to help patients understand and manage their disease and comorbidities, make dietary and other lifestyle changes, and close gaps in care. This can slow progression to kidney failure, giving patients more time to make informed decisions about the dialysis modality that’s best for them.
When a patient is progressing towards ESKD, Interwell works with them to select a treatment modality, assisting with steps like transplant preparation, dialysis training, surgical consults, and access placement. “Our coordination team supports the patients to ensure a smooth transition to ESKD,” Ketchersid said.
All of this education and planning add up. Consider Ryan, our earlier patient. As an Interwell member, he received the support required for a smooth, planned transition to dialysis and his health plan realized material savings.
Helping nephrologists increase optimal starts
We’ve developed resources and technologies that help providers within the Interwell network educate patients and deliver care in a more coordinated and comprehensive way, leading to positive clinical outcomes like increased optimal starts.
Network practices within our government program that leveraged tools like our proprietary kidney disease education suite and embedded renal care coordinators saw significant improvements in their optimal rates – with some achieving optimal start rates as high as 86 percent.
A nephrology-specific electronic health record
Our nephrology-specific electronic health record (EHR), Acumen Epic Connect, was designed to facilitate value-based care workflows and provide nephrologists with the tools they need to manage a complex patient population.
The platform enables care teams to perform and document chronic care management and transitional care management encounters in a highly efficient and coordinated way. It also supports remote patient monitoring and has robust interoperability across different healthcare settings.
These capabilities are particularly important when patients transition from CKD to ESKD, explained Carney Taylor, MD, a nephrologist and Interwell board member. "There are numerous things that need to occur for the transition to be successful. Care coordination involving multiple team members is critical for achieving optimal patient outcomes during this transition.”
Immediate results
Taylor’s practice, Eastern Nephrology Associates, partnered with Interwell and Acumen Epic Connect in 2019. They saw immediate results: Over two years, optimal starts rose from 40 percent to 90 percent for all eligible patients in value-based care arrangements.
“We’ve been able to significantly improve the care we provide our patients”

“We’ve been able to significantly improve the care we provide our patients – and our EHR certainly plays a role in it,” Taylor said.
Provider satisfaction has also improved. Taylor recalled a recent conversation with a nephrologist in his group:
“He told me that our investment in value-based care made it easier and more fulfilling for him to do his job. He recently met with a patient who he had not seen in four months, and he was pleasantly surprised to learn that the patient – with the assistance of Interwell – had completed their kidney disease education, decided on a dialysis modality, completed the appropriate testing, and had already met with the surgeon to get a dialysis access placed. Multiple complex steps had been accomplished by the care team through coordination and collaboration. Acumen Epic Connect was essential in the process and the patient received a better outcome.”
Acumen has changed the way Eastern Nephrology thinks about EHRs entirely. “We were able to shift from the mindset of thinking of our EHR as a place to complete documentation and care for one patient to drive actionable information and plans for care across all patients.”
Care and technology
Optimal starts to dialysis have a positive impact on health outcomes and costs. By pairing nephrologist-centered resources and technology with high-touch individualized care, we’re delivering significant cost savings to our payer partners and meaningfully improving our patients’ transitions to ESKD.
Notes
- Measuring Quality in Kidney Care: An Evaluation of Existing Quality Metrics and Approach to Facilitating Improvements in Care Delivery. Journal of the American Society of Nephrology. https://pubmed.ncbi.nlm.nih.gov/32054692/
- Clinical Outcomes and Healthcare Use Associated with Optimal ESRD Starts. American Journal of Managed Care. https://www.ajmc.com/view/clinical-outcomes-and-healthcare-use-associated-with-optimal-esrd-starts
- Dialysis Costs for a Health System Participating in Value-Based Care. American Journal of Managed Care. https://www.ajmc.com/view/dialysis-costs-for-a-health-system-participating-in-value-based-care