White Paper - Medications for Managing Chronic Kidney Disease: From ACEs and ARBs to SGLT2is and GLP-1 RAs
Drs. Julie Dominguez, George Hart, and Carney Taylor discuss the potential for new and emerging therapies to transform kidney care as part of a comprehensive, patient-centric approach to slowing disease progression and improving patient outcomes.
tags
Abstract
Advances in medical research are transforming chronic kidney disease (CKD) management, offering nephrologists powerful tools to slow disease progression and improve patient outcomes. This white paper explores the evolving landscape of CKD treatments, focusing on the integration of new therapeutic options such as sodium-glucose co-transporter-2 (SGLT2) inhibitors and glucagon-like peptide-1 receptor agonists (GLP-1 RAs). These medications provide significant benefits, including enhanced glycemic control, renal protection, and improved cardiovascular health. They also hold the potential to improve renal function and delay or even prevent the onset of end-stage kidney disease (ESKD). By adopting personalized, evidence-based approaches and innovative therapies, clinicians can revolutionize care for their patients living with CKD.
Introduction
More than 37 million Americans in the United States are living with some stage of CKD, though 90 percent of them are unaware they have it.1 Chronic kidney disease (CKD) is often referred to as a “silent killer” because most people with the disease do not develop symptoms until later stages when kidney function has already declined.
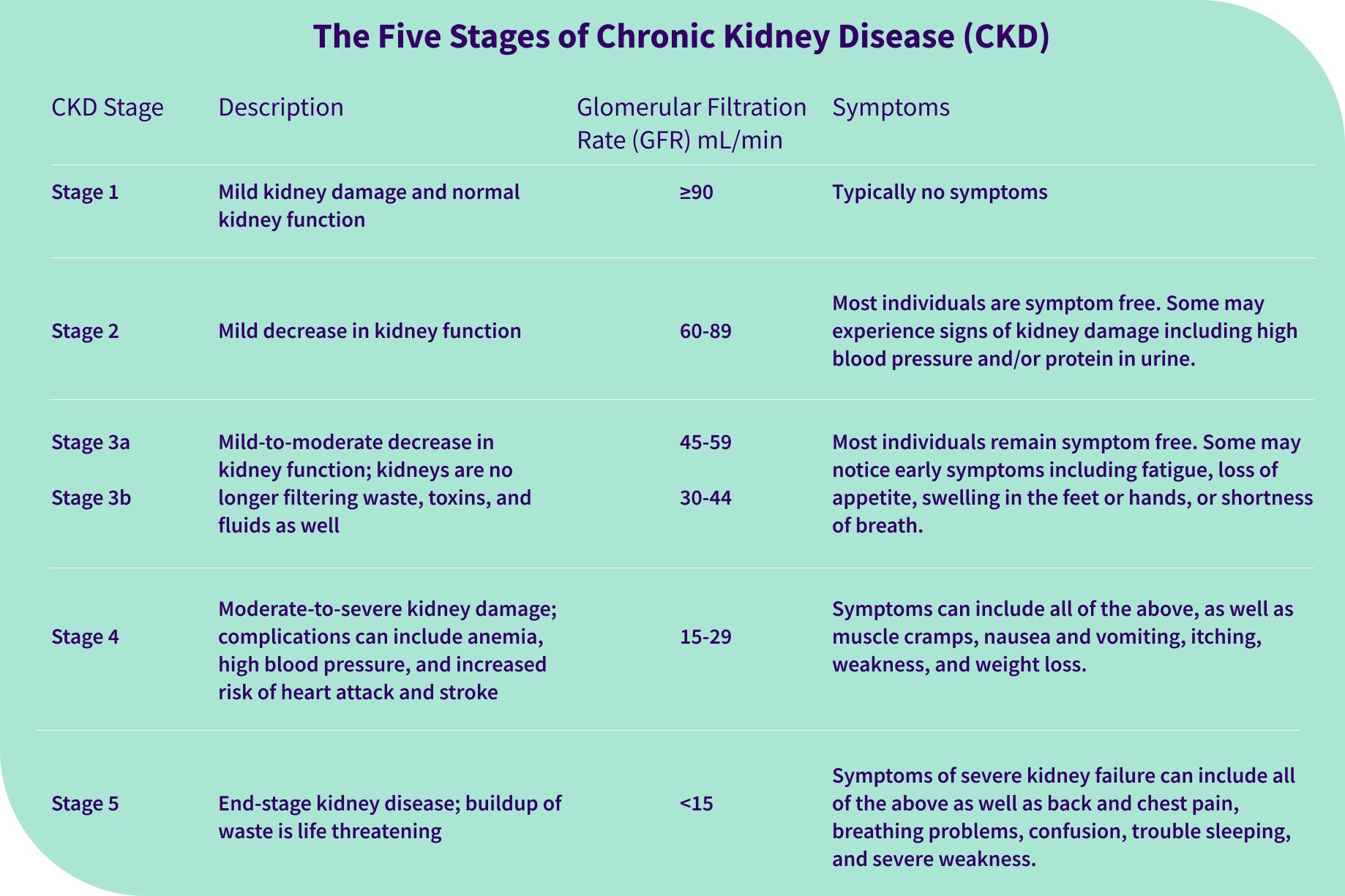
As kidney function declines, the kidneys gradually lose their ability to effectively filter waste and extra fluid from the blood. Kidney disease manifests with abnormal urine protein levels and, ultimately, with a reduced glomerular filtration rate (GFR), a standard way of measuring kidney function. Associated symptoms include fatigue, poor appetite, swelling, and shortness of breath. Left untreated, kidney disease eventually leads to kidney failure, which is treated with a kidney transplant or dialysis. Worsening CKD can also aggravate additional health issues such as diabetes, hypertension, and heart disease.
CKD is a lifetime diagnosis and kidney damage is generally irreversible. Importantly, however, CKD progression and prevention strategies including early detection, education, and proactive treatment can delay or even prevent kidney failure, extending the time until a patient needs a transplant or dialysis.
Today, nephrologists have more tools than ever to slow the progression of CKD. There are clearly established and regularly updated guidelines for keeping CKD in check through diet, lifestyle changes, medications, and managing other conditions such as diabetes. In addition, there is a growing body of evidence to show the effectiveness of therapies such as sodium-glucose co-transporter-2 (SGLT2) inhibitors and glucagon-like peptide-1 receptor agonists (GLP-1 RAs) for treating CKD.
Slowing disease progression not only improves quality of life and outcomes for people with CKD; it can also contribute to significant cost savings in CKD treatment and management. The estimated costs of managing CKD increases by stage, ranging from an average of $25,328 per person per year (PPPY) for Medicare beneficiaries with CKD stage 3 to $36,510 PPPY for beneficiaries with stages 4-5 CKD.2 Researchers estimate just a one percent reduction in the incidence of patients progressing to dialysis can save a health plan approximately $52 million in dialysis initiation costs and $30 million in each subsequent four-month cycle.3
Understanding Chronic Kidney Disease
CKD is more common among adults aged 65 or older, and in the U.S. it is slightly more common in women than in men. There are a number of chronic risk factors for CKD, including diabetes, high blood pressure, obesity, and heart disease.
The leading causes of kidney disease: diabetes and hypertension
A staggering one in three adults with diabetes also has CKD.4 Poor diabetic control and persistently elevated blood sugars over time result in inflammation leading to irreversible kidney fibrosis, which is a major pathological feature of CKD.
High blood pressure is also a major risk factor for kidney disease and as many as one in five people with high blood pressure also has kidney disease.5 High blood pressure can have a negative impact on kidney function by increasing the force of blood pushing against blood vessels throughout the body, including in the kidneys. Over time, this pressure damages the blood vessel walls, causing them to narrow and reducing blood flow, which leads to a reduced GFR and impairment of the kidneys’ ability to eliminate waste. As kidney function declines and the kidneys lose their ability to remove extra fluid from the body, an individual’s high blood pressure symptoms may worsen, resulting in a vicious cycle of deteriorating health.
Social determinants of health in CKD
Social and environmental factors such as food insecurity, housing instability, and lack of transportation can increase the risk of developing kidney disease and create barriers to care and treatment for patients with CKD. Communities of color are disproportionately impacted by social determinants of health (SDoH), contributing to poor outcomes. CKD prevalence is higher among Black adults (20 percent) than in any other group, and the prevalence of ESKD is nearly four times higher among Black adults compared to white adults.6
CKD prevalence
According to the United States Renal Data System (USRDS) 2024 Annual Data Report, overall CKD prevalence in the U.S. has remained stable over the last nearly two decades.7 Data from the Centers for Medicare & Medicaid Services (CMS) paint a less promising picture, showing that the rate of CKD diagnosis among Medicare patients rose from 13.6 to 15.4 percent from 2016 to 2022.8
It is important to keep an eye on the incidence of CKD, as growing obesity and diabetes epidemics put more people at risk of eventually developing kidney disease. Globally, kidney disease prevalence is on the rise, and it is now the seventh leading risk factor for mortality worldwide.9
Chronic Kidney Disease Progression
There are five stages of CKD, starting with mild kidney damage and no symptoms at stage 1 and progressing to CKD stage 5, at which point the kidneys are failing and patients have severe symptoms.
Unfortunately, kidney disease is often not diagnosed until later stages when symptoms first appear, with as many as one in three adults with severe CKD unaware they have the disease.x By the time many patients finally see a nephrologist, they have already progressed to Stage 4 or 5. At this stage, it is critical for healthcare providers to take proactive steps to prevent further kidney damage while preparing patients for a transition to ESKD management—either a transplant, dialysis, or active medical management without dialysis.
Current CKD Treatment Strategies
During the early stages of CKD, a typical treatment plan focuses on managing comorbidities, including controlling blood pressure and blood sugar levels, and lifestyle modifications such as following physical activity guidelines, maintaining a healthy weight, smoking cessation, and adhering to a nutritious, kidney-friendly diet.11
CKD diet and medication management
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) recommends people with CKD limit their intake of sodium to 2,300 mg per day to help control blood pressure.12 Studies show a low-protein diet high in fruits and vegetables minimizes the amount of acid to be managed by the kidneys to help reduce kidney damage13 and adequate fiber intake can also help preserve kidney function.14 People with CKD must also manage their potassium, calcium, and phosphorus levels.
Medication and supplement management is also important. For instance, people with CKD should avoid nephrotoxins such as nonsteroidal anti-inflammatory drugs (NSAIDs) that can progressively reduce how well kidneys filter out waste.15
Therapeutic interventions for CKD
Historically, therapeutic interventions for CKD focused on treating symptoms, managing associated comorbidities, and preventing further health complications. ACE (angiotensin-converting enzyme) inhibitors and ARBs (angiotensin receptor blockers), which are prescribed primarily to treat hypertension, were the first categories of drugs shown to slow CKD progression16. They have also shown benefits in CKD by lowering blood pressure and reducing excess protein in the urine, a risk factor for the progression of kidney disease.17
Diuretics are also often used to reduce volume overload by promoting the loss of water and sodium in the urine.18 Studies have shown that the group of diuretics called mineralocorticoid receptor antagonists (MRAs), which are used in combination with other drugs to manage chronic heart failure, may also help reduce the need for renal replacement therapy (RRT) for patients with CKD.19 A newer class of non-steroidal MRAs has shown significant effects on reducing albuminuria (abnormally high levels of the protein albumin in the urine), slowing the risk of progression of kidney disease, and reducing cardiovascular events in patients with diabetic kidney disease.20
Recently, diabetic drugs such as SGLT2 inhibitors and GLP-1 RAs have emerged as transformative CKD treatment options for primary care doctors and nephrologists to manage their patients. Both drug classes have demonstrated efficacy in slowing CKD progression and minimizing the risk of kidney failure, marking an exciting advance in CKD management and offering new hope for improved outcomes.
The Benefits of SGLT2 Inhibitors in Kidney Disease
In 2013, the U.S. Food and Drug Administration (FDA) approved the first SGLT2 inhibitor for the treatment of type 2 diabetes.21 While the initial indication for SGLT2 inhibitor medications was to manage blood glucose in type 2 diabetes, their benefits have proven far-reaching. Based on the latest evidence, nephrology guidelines recommend SGLT2 inhibitors as first-line treatment for patients with CKD, especially those with diabetes and/or heart failure.22 Current SGLT2 inhibitors include canagliflozin (marketed as Invokana), dapagliflozin (Farxiga), empagliflozin (Jardiance), bexagliflozin (Brenzavvy), and ertugliflozin (Steglatro).23
SGLT2 inhibitors’ mechanism of action
SGLT2 is a transporter that reabsorbs glucose from the kidneys and returns it into the blood, potentially contributing to elevated glucose levels, diabetes, and diabetic CKD. SGLT2 inhibitors work by blocking SGLT2 activity, promoting the loss of glucose and sodium in the urine rather than reabsorbing it back into the blood, resulting in lower blood sugar levels, improved kidney filtration, and lower albuminuria—helping to protect the kidneys from further damage. In addition, SGLT2 inhibitors have a diuretic-like effect that helps mitigate fluid overload, a common complication in CKD patients.
Clinical trials evaluating use of SGLT2 inhibitors in CKD
Several seminal clinical trials provide compelling evidence of the benefits of SGLT2 inhibitors in CKD.
- The CREDENCE trial found SGLT2 inhibitors reduced the risk of kidney failure and cardiovascular events among patients with type 2 diabetes and CKD.24
- The DAPA-CKD trial provided further evidence of SLGT2 inhibitors’ efficacy in treating CKD with or without type 2 diabetes, finding their use led to a lower risk of sustained decline in estimated GFR (eGFR), kidney failure, and death from renal or cardiovascular causes.25
- Lastly, EMPA-KIDNEY showed SGLT2 inhibitors led to a lower risk of kidney disease progression and hospitalization in patients with non-diabetic kidney disease and a wide range of GFRs, levels of albuminuria, and causes of CKD, broadening indications for use of SGLT2 inhibitors.26
- The results from these trials are redefining treatment standards and underscore the potential of SGLT2 inhibitors to improve quality of life for a broad spectrum of individuals with CKD.
Guidelines for use of SGLT2 inhibitors in CKD care
Though the body of evidence on SGLT2 inhibitors’ kidney benefits continues to grow, translating that evidence into actionable and accessible clinical guidelines, including use in different CKD stages and subpopulations, is critical to bridge the gap between research and clinical applications. Expanding on an earlier recommendation for the use of SGLT2 inhibitors to treat patients with type 2 diabetes and CKD, in 2024 the global nonprofit Kidney Disease: Improving Global Outcomes (KDIGO) issued an updated guideline recommending the use of SGLT2 inhibitors in adults with or without diabetes.27
The updated KDIGO guideline also notes that risks associated with SGLT2 inhibitors such as ketoacidosis and lower-limb amputations are “substantially lower than the potential absolute benefits and generally restricted to people with diabetes.”28The FDA recommends monitoring renal function before and during use of SGLT2 inhibitors, as a small percent of patients experienced renal failure after starting these medications. Other potential risks include genitourinary infections, which are seen in about 10 to 15 percent of women taking SGLT2 inhibitors, hypotension, and bone fractures.29
Future research on use of SGLT2 inhibitors in CKD care
Researchers are now studying the use of dual inhibitors of SGLT 1 and 2 such as sotagliflozin (marketed as Inpefa) on obesity and diabetes.30 In mice studies, SGLT1/2 inhibitors were shown to promote metabolic benefits and protect multiple organs affected by diabetes, including the kidneys. Further study is needed, but researchers theorize next-generation formulations such as dual inhibitors could produce even more kidney-protecting actions than the current generation of SGLT2 inhibitors. Ongoing research may also help identify candidates who will benefit most from available and emerging therapies based on genetic biomarkers and risk profiles.
A Therapeutic Game-Changer: GLP-1 Receptor Agonists for Kidney Disease
Originally developed for managing type 2 diabetes, GLP-1 RAs have since been approved for additional conditions including weight loss, reducing risk of heart problems, and treating sleep apnea. In addition, semaglutide recently became the first FDA-approved GLP-1 RA for reducing the risk of worsening kidney disease in adults with type 2 diabetes and CKD31 following results from the FLOW trial, which showed semaglutide reduced the risk of clinically important kidney outcomes and death from cardiovascular causes in this patient population.32 In addition to semaglutide (brand names Ozempic, Rybelsus, and Wegovy), current GLP-1 RAs on the market include liraglutide (Saxenda, Victoza), tirzepatide (Mounjaro, Zepbound), dulaglutide (Trulicity), exenatide (Bydureon, Bydureon BCise, Byetta), lixisenatide (Adlyxin), and albiglutide.33
GLP-1 RAs’ mechanism of action
GLP-1 RAs work by mimicking the action of endogenous GLP-1, a hormone that plays a vital role in regulating blood glucose levels by triggering the pancreas to release more insulin to help manage blood sugar, which is critical for slowing CKD progression in patients with comorbid diabetes. The drugs also produce a satiety effect that reduces appetite and food intake, resulting in weight loss, which can indirectly improve kidney health. In addition, GLP-1 RAs offer well-documented cardiovascular benefits, including reducing blood pressure and hypertension, that can further minimize risk factors associated with worsening kidney disease.34
Clinical trials evaluating use of GLP-1 RAs in CKD
Beyond indirectly slowing CKD progression by helping to manage comorbidities, emerging data suggest GLP-1 RA medications may also exhibit direct renal protective effects, with clinical studies showing patients treated with GLP-1 RAs have a lower risk of eGFR declining.35 GLP-1 RAs have also been shown to reduce inflammation and oxidative stress, or excess levels of free radicals in the body, which is a major factor in deteriorating kidney function. In addition, similar to SGLT2 inhibitors, GLP-1 RAs can also cause natriuresis, or increased urinary excretion of sodium, to regulate sodium balance and help protect the kidneys.36 These findings support the use of GLP-1 RAs as part of a comprehensive strategy to mitigate CKD progression while managing known CKD risks.
Guidelines for use of GLP-1 RAs in CKD care
The role of GLP-1 RAs in kidney care is evolving as ongoing studies investigate the expanded potential for this new class of medications, including complementary benefits when used alongside standard CKD therapies. Recent guidelines from the American Diabetes Association (ADA) and KDIGO now recommend GLP-1 RAs as first-line therapies in patients with type 2 diabetes and CKD who require additional glycemic control or cardiovascular risk reduction.37
When prescribing GLP-1 RA medications, healthcare providers should consider the patient’s disease stage, as well as comorbid conditions, drug-drug interactions, and potential risks. Adverse effects associated with GLP-1 RAs include gastrointestinal symptoms such as nausea and vomiting and a rare potential risk of pancreatitis. GLP-1 RAs are considered generally safe and effective in CKD stages 1-3, but data is limited on use in severe CKD.
Future research on use of GLP-1 RAs in CKD care
Ongoing research is underway to evaluate the effectiveness and risks of GLP-1 RAs across patient populations and possible health outcomes. A meta-analysis of data from the U.S. Department of Veterans Affairs found GLP-1 RAs were associated with a wide range of potential benefits, including reduced risk of substance abuse, cardiometabolic disorders, infectious illnesses, and several respiratory conditions. To note, the researchers also found the drugs are associated with an increased risk of conditions including hypertension and interstitial nephritis, or kidney inflammation, which are both risk factors for kidney disease.38 Further research is needed to fully understand the benefits and risks of GLP-1 RAs in patients with CKD.
Early Intervention is Critical to Realize the Potential of New CKD Medications
CKD represents a significant challenge to modern healthcare—largely due to its silent progression and late-stage detection for many patients. Our understanding of CKD’s complexities, however, has evolved and pharmacological advancements in kidney disease have ushered in a new era of CKD care, offering substantial benefits in slowing disease progression and managing associated comorbidities. Today, clinicians have access to a diverse therapeutic arsenal, including proven treatments like ACE inhibitors and ARBs and groundbreaking medications such as SGLT2 inhibitors and GLP-1 RAs that offer significant promise.
With this new wave of therapies proven to effectively slow progression of CKD, providers should note one universal takeaway: early intervention with kidney disease-specific treatment is key. These newer drugs, which may be combined with older options, are most effective when introduced before irreversible kidney damage has occurred.
Identifying CKD in its initial stages allows for timely intervention, which can preserve kidney function and significantly prevent or slow disease progression to late-stage CKD. Addressing CKD at an early stage also equips healthcare providers and patients with the tools needed to tackle the underlying causes of CKD and better manage contributing factors such as obesity, hypertension and diabetes.
Therapeutic interventions work best when part of a comprehensive care strategy
In addition to the availability of promising new therapies, innovations in care delivery and care models are also transforming CKD management and improving outcomes for patients living with CKD. It is now widely acknowledged that patients benefit most from a holistic approach that focuses on prevention, early intervention, and comprehensive, interdisciplinary care management rather than reactive, episodic treatments. Increasingly, healthcare providers and health plans are adopting value-based kidney care models that enable this proactive, patient-centered approach to care that addresses not just the disease but also the broader needs of the individual.
Clinicians, researchers, health insurance companies, public health leaders, and policymakers must work together to ensure more patients have access to CKD treatment and comprehensive care. This includes implementing efficient, widely accessible screening tools, continuing education for healthcare providers and patients, and fostering public awareness about CKD risk factors and prevention.
By leveraging new tools and approaches, we have the potential to transform the trajectory of CKD management. Now is the time to act—to identify patients earlier, provide comprehensive and proactive care, and empower individuals to take control of their kidney health.
For additional resources to help improve care and outcomes for patients with kidney disease, visit interwellhealth.com/what-we-offer.
Authors
Julie Dominguez, MD is medical director at Interwell Health, a leading value-based kidney care provider. She held prior roles as assistant clinical professor at University of California San Diego, as an associate program director for an internal medicine residency program, and in private practice. Dr. Dominguez received her MD at the University of Texas at Southwestern Medical Center, completed her Internal Medicine residency at Duke University, and went on to complete her nephrology fellowship at the University of California San Diego.
George Hart, MD spent 30 years as a practicing physician before joining Interwell Health, where he serves as chief medical officer. Prior to Interwell, he was president of Metrolina Nephrology Associates in Charlotte, North Carolina, where he led a practice of 80 providers. Dr. Hart has specialized in transplant nephrology and previously served as the medical director for the kidney and pancreas transplant programs at Carolinas Healthcare system (now Atrium Health) and as a clinical assistant professor at UNC Chapel Hill. He earned his MD from Wake Forest University.
Carney Taylor, MD, MBA has more than 20 years of clinical experience as a leading nephrologist who previously served as co-president of Eastern Nephrology Associates in North Carolina before joining Interwell Health as associate chief medical officer. Dr. Taylor is double board certified in nephrology and internal medicine. He holds a degree from East Carolina University School of Medicine, an MBA from East Carolina University, and a BA from Virginia Military Institute. Dr. Taylor completed his residency and fellowship in nephrology at Vanderbilt University.
References
______________________________________________
- National Kidney Foundation: 37 Million American Adults Now Estimated to Have Chronic Kidney Disease. 37 Million American Adults Now Estimated to Have Chronic Kidney Disease | National Kidney Foundation
- USRDS 2024 Annual Report: Healthcare Expenditures for Persons with CKD. https://usrds-adr.niddk.nih.gov/2024/chronic-kidney-disease/6-healthcare-expenditures-for-persons-with-ckd
- American Journal of Managed Care: Medical Costs for Managing Chronic Kidney Disease and Related Complications in Patients with Chronic Kidney Disease and Type 2 Diabetes. https://www.ajmc.com/view/medical-costs-for-managing-chronic-kidney-disease-and-related-complications-in-patients-with-chronic-kidney-disease-and-type-2-diabetes
- CDC: Risk Factors for Chronic Kidney Disease. https://www.cdc.gov/kidney-disease/risk-factors/index.html
- CDC: Risk Factors for Chronic Kidney Disease. https://www.cdc.gov/kidney-disease/risk-factors/index.html
- American Journal of Kidney Diseases: Genetics and ESKD Disparities in African Americans. https://www.ajkd.org/article/S0272-6386(19)30857-1/abstract
- USRDS 2024 Annual Data Report: CKD in the General Population. https://usrds-adr.niddk.nih.gov/2024/chronic-kidney-disease/1-ckd-in-the-general-population
- CKD Spotlight: Rates of CKD Diagnosis. https://ckdspotlight.healthcostinstitute.org/dashboard?cohort=CKD&payer=Traditional+Medicare#rates-of-diagnosis
- Nature: Chronic kidney disease and the global public health agenda: an international consensus. https://www.nature.com/articles/s41581-024-00820-6
- CDC: Chronic Kidney Disease in the United States, 2023. https://www.cdc.gov/kidney-disease/php/data-research/index.html
- Kidney360: Modifiable Lifestyle Behaviors and CKD Progression: A Narrative Review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9136893/
- NIDDK: Slow Progression & Reduce Complications. https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-management/kidney-disease/identify-manage-patients/manage-ckd/slow-progression-reduce-complications
- Journal of Renal Nutrition: Reducing the Dietary Acid Load: How a More Alkaline Diet Benefits Patients With Chronic Kidney Disease. https://pubmed.ncbi.nlm.nih.gov/28117137/
- Toxins: The Role of Dietary Fiber and Gut Microbiome Modulation in Progression of Chronic Kidney Disease. https://pmc.ncbi.nlm.nih.gov/articles/PMC8955792/
- International Journal of Clinical Pharmacy: Kidney function and use of nonsteroidal anti-inflammatory drugs among elderly people: a cross-sectional study on potential hazards for an at risk population. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6132969/
- National Kidney Foundation: ACE & ARBs - Uses, types, effectiveness, side effects. https://www.kidney.org/kidney-topics/ace-inhibitors-and-arbs
- Cleveland Clinical Journal of Medicine: ACE inhibitors and ARBs: Managing potassium and renal function. https://www.ccjm.org/content/86/9/601
- Nature Reviews Nephrology: Diuretics in patients with chronic kidney disease. https://www.nature.com/articles/s41581-024-00918-x
- Hypertension: Mineralocorticoid Receptor Antagonist Use and Hard Renal Outcomes in Real-World Patients With Chronic Kidney Disease. https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.121.18360
- BMC Nephrology: Finerenone in the management of diabetes kidney disease. https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-025-03985-9
- NIDDK: Story of Discovery: SGLT2 inhibitors: harnessing the kidneys to help treat diabetes. https://www.niddk.nih.gov/news/archive/2016/story-discovery-sglt2-inhibitors-harnessing-kidneys-help-treat-diabetes
- National Kidney Foundation. SGLT2 inhibitors. https://www.kidney.org/kidney-topics/sglt2-inhibitors
- Drugs.com: List of SGLT-2 inhibitors (sodium-glucose cotransporter-2 inhibitors). https://www.drugs.com/drug-class/sglt-2-inhibitors.html
- New England Journal of Medicine: Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. https://www.nejm.org/doi/full/10.1056/NEJMoa1811744
- New England Journal of Medicine: Dapagliflozin in Patients with Chronic Kidney Disease. https://www.nejm.org/doi/full/10.1056/NEJMoa2024816
- New England Journal of Medicine: Empagliflozin in Patients with Chronic Kidney Disease. https://www.nejm.org/doi/full/10.1056/NEJMoa2204233
- KDIGO: KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. https://kdigo.org/wp-content/uploads/2024/03/KDIGO-2024-CKD-Guideline.pdf#page=99
- KDIGO: KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. https://kdigo.org/wp-content/uploads/2024/03/KDIGO-2024-CKD-Guideline.pdf#page=101
- Federal Practitioner: Risks vs Benefits for SGLT2 Inhibitor Medications. https://pmc.ncbi.nlm.nih.gov/articles/PMC6368009/
- Diabetes Care. Sotagliflozin, a Dual SGLT1 and SGLT2 Inhibitor, as Adjunct Therapy to Insulin in Type 1 Diabetes. https://pmc.ncbi.nlm.nih.gov/articles/PMC4831906/
- Pharmaphorum: Ozempic is first GLP-1 FDA-approved for kidney disease. https://pharmaphorum.com/news/ozempic-first-glp-1-drug-fda-approved-kidney-disease
- New England Journal of Medicine: Effects of Semaglutide on Chronic Kidney Disease in Patients with Type 2 Diabetes. https://www.nejm.org/doi/full/10.1056/NEJMoa2403347
- Drugs.com. GLP-1 Agonists: List of Medications for Diabetes and Weight Loss. https://www.drugs.com/drug-class/incretin-mimetics.html
- Frontiers in Clinical Diabetes and Healthcare: The benefits of GLP1 receptors in cardiovascular diseases https://www.frontiersin.org/journals/clinical-diabetes-and-healthcare/articles/10.3389/fcdhc.2023.1293926/full
- American Journal of Kidney Diseases: Kidney and Cardiovascular Outcomes Among Patients With CKD Receiving GLP-1 Receptor Agonists: A Systematic Review and Meta-Analysis of Randomized Trials https://www.ajkd.org/article/S0272-6386(25)00042-3/fulltext
- Kidney Research and Clinical Practice: GLP-1 receptor agonists in diabetic kidney disease: current evidence and future directions. https://krcp-ksn.org/journal/view.php?doi=10.23876/j.krcp.22.001
- ACP Diabetes Monthly: ADA, KDIGO offer consensus statements on managing diabetes and chronic kidney disease https://diabetes.acponline.org/archives/2022/10/14/1.htm
- Nature Medicine: Mapping the effectiveness and risks of GLP-1 receptor agonists. https://www.nature.com/articles/s41591-024-03412-w