Empowering Patients, Reducing Costs: Patient Engagement Strategies for Sustainable Value-Based Kidney Care
In value-based care models, patient engagement strategies can increase member satisfaction, improve outcomes, and reduce the costs of managing chronic kidney disease.
tags

Success in a value-based care model is highly dependent on the engagement level of the patients at its center. While patient-centered care is the gold standard for healthcare delivery, its potential is only realized when patients become active partners in their health journey. Understanding and fostering this partnership not only improves patient satisfaction but also directly impacts long-term outcomes and total cost of care.
Why payers must prioritize patient engagement for chronic kidney disease
For health plans, the growing population with chronic kidney disease (CKD) and end-stage kidney disease (ESKD) represents a perfect storm of rising costs and declining member health. The number of people with kidney disease is already substantial and continues to expand, placing an enormous financial and operational burden on payers.
The growing burden of chronic kidney disease:
- CKD affects one in seven U.S. adults. Nearly a third of people with diabetes and one in five people with high blood pressure have kidney disease.1
- Managing care for members with CKD historically costs twice that of managing care for those without the disease, regardless of insurer.2
- Spending on older adults with stages 4–5 CKD is more than $36,000 per person per year (PPPY).3
- Approximately 15 percent of patients have never seen a nephrologist before reaching ESKD.4 When they finally do, it is often too late to meaningfully slow disease progression.
- Once patients progress to ESKD—at which point many initiate costly dialysis treatments—the cost of managing their care skyrockets to upward of $100,000 PPPY.5
These statistics paint a stark picture of system in need of change. Without proactive healthcare interventions and meaningful engagement with their own care, patients are left to navigate a complex illness with inadequate support, leading to poor outcomes and significant, often avoidable, costs. By implementing effective patient engagement strategies, payers can empower patients, ensure timely access to specialist care, and promote optimal treatment paths, ultimately reducing the immense financial strain of kidney disease and improving population health.
The challenges of improving patient engagement in chronic care
Engaging patients, especially those with complex chronic conditions like CKD, presents a unique set of challenges. Patients often manage multiple comorbidities, such as heart disease and diabetes, requiring them to interact with a wide array of specialists. As Interwell Health Associate Chief Medical Officer Dr. Carney Taylor pointed out during a sponsored webinar with AHIP, CKD patients are often asked to prioritize certain aspects of their health or care team interactions, leading to missed opportunities for holistic care.
Barriers to effective patient engagement:
- Lack of disease awareness: Kidney disease often has no symptoms until patients reach kidney failure. Many individuals are unaware of their condition or may have been told something is off in their labs but lack the context to realize the significance of these results. Yet understanding a CKD diagnosis is a critical first step to preventive action.
- Mistrust in the healthcare system: Patients may be hesitant to engage with programs and suspicious of unsolicited calls offering benefits or resources, especially if the program wasn’t recommended by their primary care provider (PCP).
- Social determinants of health (SDoH): Financial stressors, unstable housing, or lack of access to transportation can force patients to prioritize basic needs over their health management.
- Logistical hurdles: Outdated contact information, language barriers, and patient reluctance to answer unknown numbers make initial contact a significant operational challenge.
Overcoming these barriers requires deliberate and multifaceted patient engagement strategies, starting with building a foundation of trust.
Proven patient engagement strategies for better outcomes
A successful patient engagement program balances standardized processes with the flexibility to personalize care. It's about meeting patients where they are and creating value from the very first interaction.
1. Trust building: The first step in patient engagement
Initial contact is a critical moment. Many patients are wary of unrecognized phone numbers, so a multi-modal outreach approach—using phone, email, and mail—is important until the patient’s preferred method of communication is identified. Once a patient is enrolled in an engagement program such as Interwell 360, a care team member can perform a virtual initial assessment to collect basic health information, demographics, and knowledge of existing care team members.
“Most importantly, we want to assess the patient’s current needs and how we can create value for them immediately, while also weaving in bits and pieces of education,” says Jessica Demaline, senior vice president of healthcare operations at Interwell. “Our goal is to make sure that the patient answers our phone call the next time that we call and wants to have additional conversations with our interdisciplinary care team.”
2. Personalized care: Meeting patients where they are
Every patient is different. Some may be in denial due to fear, while others are simply unaware of their treatment options. Some may be grappling with social determinants of health hardships, such as lack of transportation, or behavioral health challenges. An effective engagement team must be agile enough to identify and address these individual needs.
Once an initial connection is made, the goal is not to overwhelm but to build rapport and trust through ongoing education and coaching. Interwell renal care coordinators (RCCs) often find success by starting with casual, supportive check-ins: "How has your blood pressure been?" or "How have you been feeling?" This light, conversational approach makes patients feel supported, rather than scrutinized. From there, it’s possible to move into longitudinal care management, such as medication adjustment and dietary guidance, and episodic care management when needed, such as when a patient’s blood sugar levels spike.
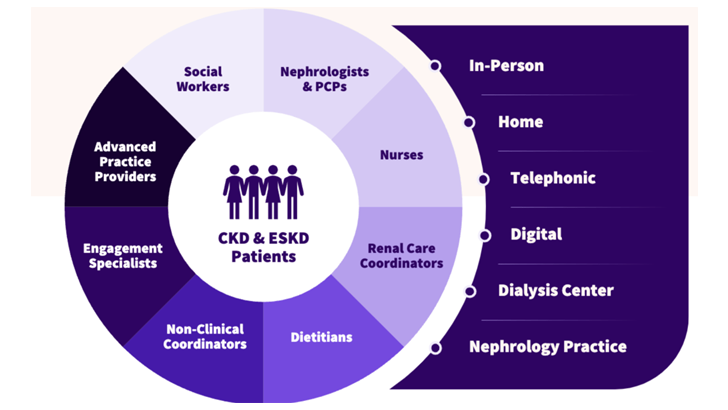
3. Interdisciplinary care team: A collaborative approach to CKD care
True patient-centered care involves a holistic team. In value-based models, CKD patient care often includes nephrologists, advanced practice providers (APPs), nurses, dietitians, social workers, care coordinators, and non-clinical coordinators. This team works together to address the whole person, not just the disease. This can include making connections to local nephrologists, assisting with transportation, reviewing medications, and conducting timely post-hospitalization outreach.
Alice, a grandmother and retired medical transcriptionist from Pueblo, Colorado, calls her Interwell 360 extended care team her "kidney club.” Diagnosed with high blood pressure and near kidney failure, Alice began meeting with an Interwell registered dietitian, nurse, and social worker. “Interwell made me feel like they were sitting down at the kitchen table with me and a cup of coffee,” said Alice. “I think of them as my guardian angels. A lot of the things that the dietitians and the nurses have taught me are actually easier than the way I was doing it before.”
This comprehensive support, addressing both clinical needs and social determinants of health, empowers patients like Alice to feel in control of their health.
The measurable benefits of patient engagement
When patients are actively invested in their health, the positive impacts are clear and quantifiable. Patient engagement is associated with improved adherence to treatment plans and higher performance on CAHPS surveys and Medicare Advantage Star ratings. Furthermore, connecting patients with the right resources at the right time can prevent costly and avoidable healthcare events.
One study found patient engagement, as measured by the Patient Activation Measure, was associated with better health outcomes including an increase in healthy behaviors, greater use of preventive screening tests, and lower costs.6 An Interwell analysis reinforces the strong correlation between engagement and improved outcomes among the kidney patient population. Data from more than 10,000 patients aligned with one payer partner shows higher engagement led to positive results including:
- 12 percent reduction in total cost of care
- 15 percent reduction in all-cause hospitalizations
In addition, by engaging patients in a wraparound care program, Interwell achieved a 34 percent increase in the percentage of patients followed by a nephrologist after 15 months of partnership with one health plan. This metric is notable, as early referral to a nephrologist is associated with slowed disease progression, reduced hospitalizations, and reduced mortality.
Engaged patients are also more likely to use additional resources, creating a virtuous cycle of improved outcomes. “We have a big toolbox of resources, support, and education that we can offer to patients. But if patients don’t engage with us, they really can’t reap those benefits,” says Dr. Julie Dominguez, medical director of Interwell Medical Group. “The good news is, once patients engage with us, we know that we decrease total cost of care and admissions, and we help patients engage with their healthcare teams and their own care a lot more.”
Using digital health engagement to enhance care
Human interaction is the cornerstone of effective patient engagement, often revealing patient risk factors that algorithms can’t capture. Yet technology—including digital health engagement tools, advanced analytics, and AI—can be powerful enablers that allow care teams to work more efficiently and proactively.
How digital tools, predictive analytics, and AI help care teams deliver better CKD outcomes:
- Predictive analytics: By analyzing claims, electronic health record (EHR), and health information exchange (HIE) data, risk stratification models can predict a patient's risk of hospitalization or CKD progression. This allows care teams to prioritize outreach to the highest-risk individuals who need support most urgently. For instance, Interwell uses machine learning tools to accurately predict risk and flag patients for timely clinical interventions, contributing to improved outcomes including 20 percent fewer all-cause hospitalizations than the national average.
- AI-powered insights: Ambient listening and other AI tools can enable fast, accurate clinical documentation, efficient patient note sharing, and clinical decision support. For instance, Interwell uses AI-generated call summaries and automated information retrieval to deliver recommended interventions to care team members. These tools reduce the burden of pre-call preparation, after-call documentation, and manual notetaking, increasing caregiver efficiency and empowering care team members to focus on effective patient engagement and interventions.
- Sentiment analysis: AI can also process large volumes of data to determine patient preferences at population scale. For instance, by analyzing tens of thousands of enrollment call transcripts using proprietary large language models (LLMs), Interwell’s data team discovered that less-scripted, more interpersonal conversations with repetition and simplicity led to higher engagement.
- Secure patient messaging: Patient communication tools help care teams focus on understanding and addressing patients' needs and fostering more meaningful interactions. For instance, many nephrology practices use the Epic MyChart patient portal available through Acumen Epic Connect, the most broadly adopted nephrology specific EHR, to securely interact with patients.
- Healthcare engagement tools: Patient education platforms such as Interwell Learning provide patients with short, easy-to-understand educational segments, often delivered through their local nephrologist’s office. This reinforces learning and strengthens the patient-provider partnership.
A partnership for success in value-based care
In the shift to value-based care, improving patient engagement is a strategic imperative for payers to foster trust, increase care plan adherence, and ensure timely interventions that can delay disease progression and enhance overall health outcomes while lowering healthcare costs. Collaboration with a value-based care partner can significantly improve patient engagement by leveraging their expertise in proactive care coordination, personalized patient outreach, and resource alignment to address the unique needs of CKD and ESKD patients.
Best practices for optimizing patient engagement in value-based care partnerships:
- Timely data sharing: Accurate and up-to-date patient data—from demographics to hospital admissions—is crucial for timely outreach and intervention.
- Co-branded communication: When payers introduce a value-based care partner to members through a primer letter, it builds credibility and trust. Co-branded materials reinforce that the program is a legitimate and valuable benefit.
- Aligned care management teams: When payer and value-based care management teams work in collaboration, they can ensure patients are connected to all available resources, creating a seamless and supportive experience.
- PCP education: When in-network PCPs understand the availability and benefits of kidney care management programs, they can help address common barriers to enrollment such as lack of patient awareness and trust.
Ultimately, the goal is to create a healthcare ecosystem where patients feel seen, heard, and supported. As a value-based kidney care provider, Interwell Health focuses on building trust and creating value through proven patient engagement strategies designed to delay disease progression, achieve quality metrics, and improve individual and population health outcomes while bringing down the total cost of care.
To learn more about Interwell Health’s robust patient engagement strategies and results, visit our website.
###
References
- NIH: Kidney Disease Statistics for the United States. https://www.niddk.nih.gov/health-information/health-statistics/kidney-disease
- USRDS: Healthcare Expenditures for People with CKD. https://usrds-adr.niddk.nih.gov/2022/chronic-kidney-disease/6-healthcare-expenditures-for-persons-with-ckd
- USRDS: Healthcare Expenditures for People with CKD. https://usrds-adr.niddk.nih.gov/2024/chronic-kidney-disease/6-healthcare-expenditures-for-persons-with-ckd
- USRDS: Incidence, Prevalence, Patient Characteristics, and Treatment Modalities. https://usrds-adr.niddk.nih.gov/2024/end-stage-renal-disease/1-incidence-prevalence-patient-characteristics-and-treatment-modalities
- USRDS: Healthcare Expenditures for Persons with ESRD. https://usrds-adr.niddk.nih.gov/2024/end-stage-renal-disease/9-healthcare-expenditures-for-persons-with-esrd
- Health Affairs: When patient activation levels change, health outcomes and costs change, too. https://www.healthaffairs.org/doi/10.1377/hlthaff.2014.0452